Follow-up management- remote care over ratios
Topics: Industry insights
The Problem with ratios
Many Trust executives talk about FU reduction as an essential and obvious improvement to make, they may be right but it's a complex issue and far from being black and white.
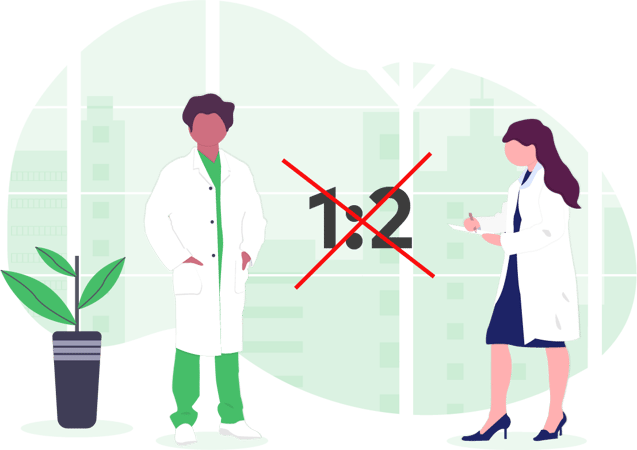
According to the long-term plan, every consultant regardless of specialty and patient cohort, should reduce their face to face follow-up activity by 30%. In order to visualise this in practice let’s assign a couple of numbers. Let’s say that to achieve this 30% reduction, you need to keep your follow-up ratio at 1:2. For every new appointment, you’re only allowed 2 follow-ups. These targets are often used as a performance indicator by the NHS (more on this here).
Now the problem with setting targets like these is that it inevitably encourages churn. If you limit the number of ‘allowed’ appointments and FU activity is cut short, the patient might end up booking a new appointment with their GP only to enter the cycle again. Another hospital appointment, and another 2 FU appointments scheduled. But this time the patient is dealing with a new consultant who has not been involved in tracking their care previously. All the previous support they received throughout their care journey disappears and the new consultant is, to an extent, forced to start the process again. This may happen once or twice or several times, and the FU target 1:2 ends up being completely arbitrary. It certainly ends up having no positive impact on the patient’s care, or cost and time implications involved.
Find the right patients to help
Before implementing remote management, it is essential to understand the nuances around different appointments and different patients and when remote healthcare is a sensible solution and when it isn’t.
The DrDoctor approach to outlining FU management projects starts with a data assessment where we see which patients are more likely to benefit from remote follow-ups. This data is then validated through a clinical assessment, led by clinicians in charge of each specialty. We normally find that for around 70% of patient cohorts within each specialty, the solution will likely work very well. This means that for 30% of patients remote management is not quite right. At least not just yet.
This allows us to target our efforts on the cohort of patients who are most likely to benefit. With that understanding we then work with the Trust to create a roadmap of how we are going to help an Outpatient department move to remote management, starting with the highest opportunity first. This means picking clinical specialties where a large number of patients are identified as potential beneficiaries. It’s important to get this right and focus on the parts of the hospital where the remote solution is going to be not only adopted but also loved by patients, in order to deliver great results.
Making the NHS sustainable
We feel there’s been a great shift towards remote care, and we think it’s fantastic as we are so proud to be a part of it. We believe the future of healthcare will gain huge value from remote management. We have also learnt a lot through our work so far, not least that there is nuance and complexity in every case – it's safe to say FU reduction is not quite as straightforward as we initially thought. When designing new solutions, the best place to start is by collaborating with the NHS and gaining a real understanding of the big picture.
We recently hosted an NHS executive workshop here in London and invited our attendees to identify some of the biggest challenges facing the healthcare services today. A number of our guests identified communication as a real issue. We could certainly relate as that is why DrDoctor exists- to help patients and hospitals communicate better with each other. Another key challenge identified in the room was the high number of follow-up (FU) appointments given out to patients. We agreed again and as such have just built a new product that focuses on streamlining remote care.
It’s clear the NHS is under immense pressure to look after all of us while honouring the original values it was set up on (such as keeping it free). It’s also clear that technology can help when done right. There’s a number of start ups like us doing our best to create slick digital solutions to make communication in the healthcare setting easier and more in-line with the world we live in where communication and connectivity exists literally at our fingertips. It’s not enough to build really good software, however. This is why when creating our follow-up management product, we started by really understanding how follow-up appointments work in the NHS. Because what you have to do is understand the real detail behind the issue.
More on our Follow-up Management product and the collaboration behind it here.